Norovirus
Norovirus infection causes gastrointestinal illness, which is an inflammation of the stomach and intestines associated with rapid onset of diarrhea and/or vomiting. This infection is sometimes referred to as the “stomach flu,” but noroviruses are not related to the flu (influenza), which is a respiratory illness caused by influenza virus. Norovirus is very contagious and tends to circulate in closed populations such as long-term care facilities and schools.
Table of Contents
What is Norovirus?
Norovirus (previously referred to as Norwalk-like virus) is a single-stranded ribonucleic acid (RNA) virus within the family Caliciviridae. Infections with norovirus are sometimes called the “stomach flu” but it is not related to the virus causing influenza. There are six major types of norovirus with one type associated with the majority of worldwide outbreaks since the mid-1990s.
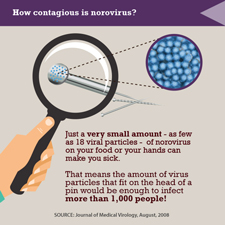
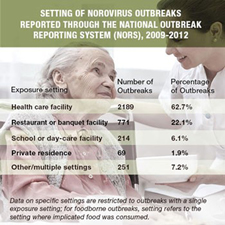
 Norovirus is very contagious and can spread quickly in closed places like daycare centers, schools, long-term healthcare facilities such a nursing homes, and cruise ships where people are in close proximity to each other. However, anyone can get infected with norovirus and you can get it more than once. One estimate is that a person will get norovirus infections about five times during their lifetime. Many people get sick with norovirus in cooler winter months because people are more likely to be indoors and in closer contact with one another. The virus is transmitted person to person, or by consuming food or water contaminated with the virus. You can become infected by accidentally getting stool or vomitus from infected people in your mouth. Direct transmission may occur through ingestion of aerosolized vomitus, and indirect transmission may occur while eating food or drink contaminated with norovirus, by having contact with an infected person such as through caring for them or sharing food or eating utensils, and through touching surfaces or objects contaminated with norovirus.
Norovirus is very contagious and can spread quickly in closed places like daycare centers, schools, long-term healthcare facilities such a nursing homes, and cruise ships where people are in close proximity to each other. However, anyone can get infected with norovirus and you can get it more than once. One estimate is that a person will get norovirus infections about five times during their lifetime. Many people get sick with norovirus in cooler winter months because people are more likely to be indoors and in closer contact with one another. The virus is transmitted person to person, or by consuming food or water contaminated with the virus. You can become infected by accidentally getting stool or vomitus from infected people in your mouth. Direct transmission may occur through ingestion of aerosolized vomitus, and indirect transmission may occur while eating food or drink contaminated with norovirus, by having contact with an infected person such as through caring for them or sharing food or eating utensils, and through touching surfaces or objects contaminated with norovirus.
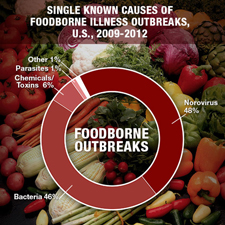
The Centers for Disease Control and Prevention (CDC) notes that norovirus is the most common cause of acute gastrointestinal illness and foodborne-related illness in the US. According to CDC, as many as 21 million illnesses are caused by noroviruses each year. Part of the reason that there are so many norovirus illnesses in the US is because it is so highly infectious: persons infected with norovirus have billions of norovirus particles in their stool but it takes few as 18 of those particles to cause illness.
The New Mexico Department of Health investigates many norovirus outbreaks every year.
Figure 1. Norovirus Outbreaks, New Mexico, 2012-2023
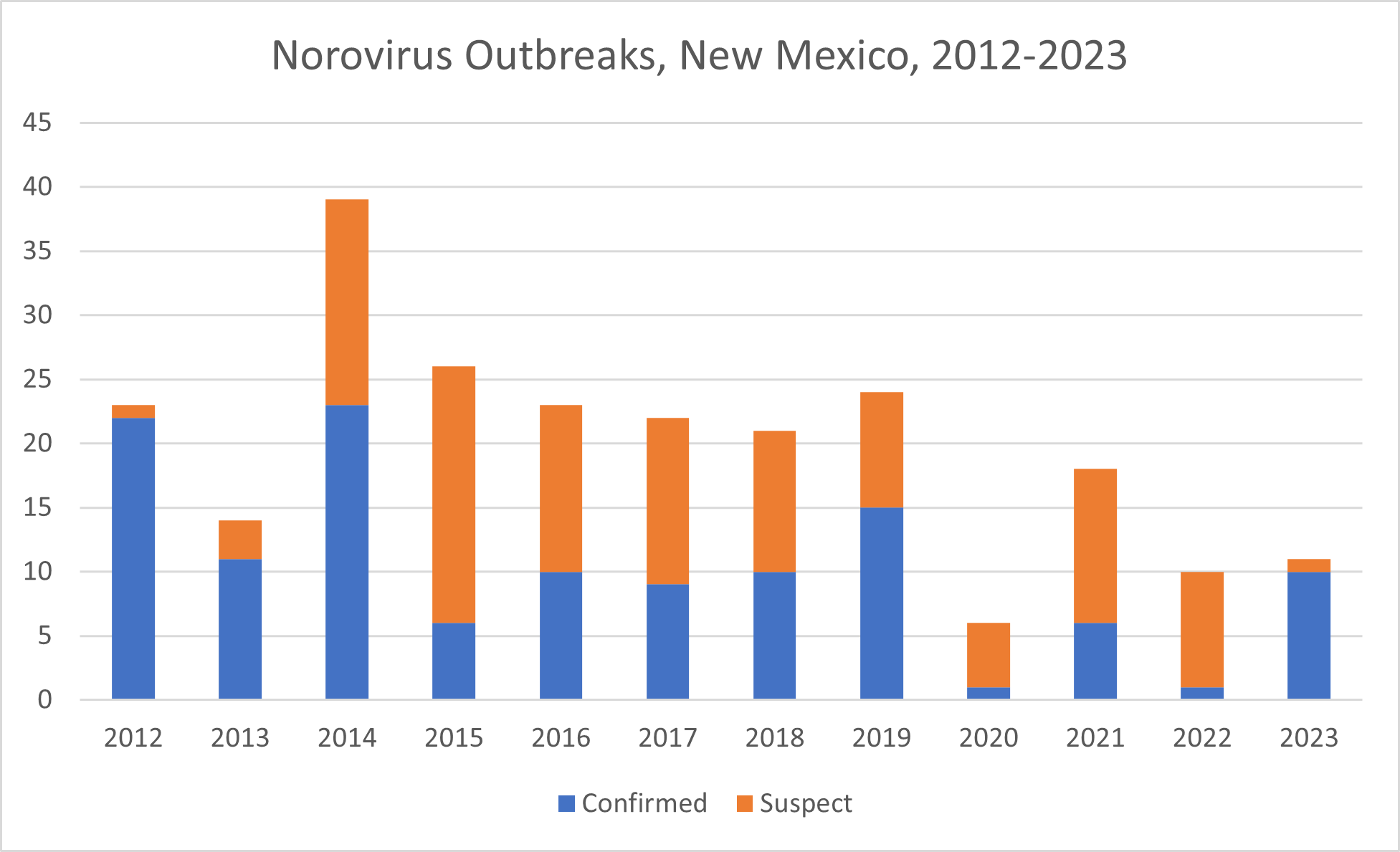
NOTE: Other includes weddings, family gatherings, restaurants, shelters, detention facilities, work environments. Outbreaks are defined as confirmed if three or more cases were laboratory confirmed to be norovirus.
The importance of norovirus in causing acute gastrointestinal illnesses has become increasingly recognized partly due to advances in laboratory testing and reporting, which has expanded the understanding of the epidemiology of norovirus infection.
Illness associated with Norovirus
People who are infected and become ill usually start feeling sick within 12-48 hours after exposure. Illness is characterized by acute onset of vomiting, watery, non-bloody diarrhea with abdominal cramps, and nausea. Body aches, fatigue, and headache are also commonly reported. Low-grade fever is present in about half of cases. Studies suggest that up to 30% of infections may be asymptomatic. Generally, medications are not needed or effective and most people recover within 1-3 days; however, the virus can be found in their stool for 2 weeks or more after their illness resolves. Very young children or older adults may have more serious illness with dehydration being the most common complication which may require intravenous replacement fluids.
Documents
- Gastrointestinal (GI) Outbreaks Toolkit for Long Term Care Facilities (LTCF)
- Outbreak Line List Template
- Prefilled Specimen Submission Form for norovirus testing (raw stool)
- Prefilled Specimen Submission Form for enteric bacteria testing (transport media)
Prevention

There is no vaccine to prevent norovirus infection. The best way to prevent infection is to wash your hands often, especially after using the toilet, changing diapers, cleaning up diarrhea or vomit, and always before eating or preparing food. Appropriate hand hygiene has been identified by CDC as the “single most important method to prevent norovirus infection”. Alcohol-based hand sanitizers are not effective against norovirus and are not a substitute for washing hands with running water and soap.
Norovirus particles also can stay on surfaces for many weeks and spread infection through contaminated objects. Disinfecting potentially contaminated surfaces is recommended to prevent exposure and further spread of norovirus. The most effective disinfectant is a chlorine bleach solution made from diluting household bleach in 1:10 dilution by mixing one cup bleach in nine cups water (or ¼ cup bleach to 2 ¼ cups of water). Healthcare settings should use Registered Hospital Disinfectants Effective Against Norovirus that are US Environmental Protection Agency (EPA) registered and labeled for use in such settings.
Clothing that is contaminated with stool or vomitus should immediately be removed and washed. Soiled items should be handled carefully-without agitating them-to avoid spreading virus. If available, wear rubber or disposable gloves while handling soiled clothing or linens and wash your hands after handling. The items should be washed with detergent at the maximum available cycle length and then machine dried at a high heat setting.
Food handlers and healthcare providers should be especially careful not to infect others. Anyone with norovirus illness, but especially food handlers (i.e., working in restaurants, facilities, catering businesses, or any venue that provides food to the public) and healthcare providers, should not work while they have symptoms and for 72 hours after they recover from their illness.
The New Mexico Department of Health does not recommend closing schools even if numerous children and/ or teachers have norovirus. Those who are sick should stay home for three days after they are feeling better and no longer have symptoms.
How can you and your family prevent getting infected with norovirus?
If you’re sick stay home.
To decrease the risk of getting a norovirus infection, the New Mexico Department of Health recommends that you:
- Wash all surfaces of your hands with soapy water for 20 seconds.
- After using the bathroom
- After changing diapers
- Before preparing foods
- Before eating
- Wash your hands more often when someone in your household is sick.
- Clean and disinfect surfaces with a 1:10 household bleach solution immediately after vomiting or diarrheal episodes.
- Avoid preparing food for others while you have symptoms and for at least three days after you recover.
Information for Healthcare Providers
Individual cases of norovirus infection are not required to be reported to the New Mexico Department of Health. However, norovirus outbreaks do require reporting under the “suspected foodborne illness in two or more unrelated persons”.
It is important in outbreaks to determine whether the cause is norovirus or from another source such as a bacterial infection. Many clinical and public health laboratories have the capability to test human specimens (stool and vomitus) for norovirus. The New Mexico Department of Health Scientific Laboratory Division (SLD) uses real-time reverse transcription polymerase chain reaction (RT-qPCR) allowing for grouping of norovirus at the genetic level (genotyping). The New Mexico Department of Health recommends at least 3-5 samples of either feces and/or vomitus be collected and submitted to the SLD for testing. It also is important to test for other pathogens, including salmonella, shigella, and other bacteria causing similar illness. If you suspect an outbreak, the New Mexico Department of Health can assist with laboratory testing and preventing further illness. Call the Reporting & Surveillance hotline at 1-833-796-8773 to report possible outbreaks and/or request assistance.
Specimen Collection
This video explains how to submit specimens to the SLD biological sciences bureau.
CaliciNet

SLD participates in the CDC CaliciNet Program. CaliciNet is an electronic norovirus outbreak surveillance network allowing certified laboratories to upload their genotyping information to a national database.
The CaliciNet database allows tracking of transmission sources and temporal spread of specific norovirus genotypes.
Control Measure Guidelines
In general, persons with suspected norovirus infection should be managed with standard precautions with careful attention to hand hygiene practices (as described below). However, contact precautions should be implemented when caring for diapered or incontinent persons, during outbreaks in a facility, and when there is the possibility of splashes that might lead to contamination of clothing.
Prophylaxis is not applicable for persons with possible exposure. Ill staff in specific positions (e.g., food handlers, childcare personnel and healthcare personnel with direct patient care duties) until a minimum of 48 hours after signs/symptoms resolve.
Cohort (i.e., group together) ill patients and/or residents in institutional settings such as long-term care facilities and hospitals until at least 48 hours after signs and symptoms fully resolve. It is ideal to cohort immunosuppressed and elderly persons for 72 hours.
Management of Norovirus in an Institutional Facility Outbreak
- Notify the New Mexico Department of Health by calling the Reporting & Surveillance hotline at 1-833-796-8773 to report the outbreak and obtain assistance. The Gastrointestinal (GI) Outbreaks Toolkit for Long Term Care Facilities (LTCF) can be useful during the outbreak. One of the most important components of monitoring the outbreak is to use the Outbreak Line List Template to conduct surveillance at the facility. The line list should be faxed to the New Mexico Department of Health daily if new cases occur. The line list includes:
- Number of ill residents
- Number of ill staff (include job function/location and residents with whom they work)
- Onset dates (and times if possible) of signs/symptoms
- Signs and symptoms
- Duration of illness
- Physical distribution of illness in the facility
- Hospitalizations/deaths
- When a single ward is affected: at a minimum, restrict admissions and discharges in the ward for a minimum of 48 hours after the resolution of the last case.
- When multiple wards are affected: restrict admissions and discharges for the entire facility for a minimum of 48 hours after the resolution of the last case.
- Collect samples (diarrhea or vomitus) for laboratory testing as necessary from people who are/have been ill, if this has not already been done. Try to obtain 3-5 specimens (or as many possible) from an outbreak in a long term care facility home or other institution.
- Provide education to facility staff about clinical presentation, disease transmission, and prevention and control measures.
- Implement all practices recommended by both the New Mexico Department of Health and the New Mexico Environment Health Food Program regarding meal services and the kitchen.
Resident-oriented Prevention and Control Measures
- Increase surveillance for diarrhea and vomiting.
- Ensure that all residents wash their hands after using the bathroom, before meals and after any episode of diarrhea or vomiting.
- Isolate ill residents from others by confining them to their rooms until 3 days after their last symptoms resolve.
- Group ill people together (cohort) if possible.
- Discontinue activities where ill and well residents would be together.
- Group activities should be kept to a minimum or ideally postponed until the outbreak is over.
- Avoid transferring residents to “sister facilities” or other institutions while cases of gastroenteritis are occurring. If a transfer is necessary, the receiving institution must be notified of the outbreak.
Staff-oriented Prevention and Control Measures
- Maintain strict hand hygiene when entering and leaving every resident room.
- Wash hands with soap and water for at least 20 seconds when entering or leaving a room.
- Alcohol-based hand sanitizers may be used when hands are not visibly soiled, though the effectiveness of these products against noroviruses is uncertain.
- Ill staff should stay home for a minimum of 48 hours after symptoms resolve.
- Staff should be assigned to work with either well residents or ill residents.
- All staff should wear gloves when caring for residents or handling bedding.
- Staff should wear masks when caring for a resident who is vomiting.
- Housekeeping staff should wear gloves and masks when cleaning contaminated or potentially contaminated surfaces or laundry.
- Ensure food staff are aware of the necessary precautions in designated food service areas and educate food staff on the importance of hand washing.
Visitor-oriented Prevention and Control Measures
- Recommend discontinuing visitation to healthcare facilities (e.g., nursing homes) until the outbreak is over. If visitation is allowed, visitors should go directly to the person they are visiting and not spend time with anyone else. They should wash their hands well upon entering and leaving the room. They should not visit if they are sick.
- Recommend posting signs to remind visitors who are sick to delay their visit until they are well, and post signs that encourage hand washing.
Management of Norovirus in a Daycare Associated Outbreak
- Exclude symptomatic children from day care until cessation of illness. Upon return, hand washing of children must be strictly monitored.
- Exclude symptomatic staff from work until at least 48 hours, or ideally 72 hours, after cessation of illness.
- Staff hand washing, especially after changing diapers and before food preparation, must be strictly enforced.
- If possible, implement a cohort system (whereby infected children and staff are placed together in a separate area away from other children and staff).
- Staff should wear gloves and masks when cleaning contaminated or potentially contaminated surfaces or laundry.
Management of Norovirus in a Restaurant or Hotel Associated Outbreak
Food handlers and preparers with gastroenteritis caused by norovirus should not work until a minimum of 48 hours, or ideally three days (72 hours), after complete resolution of signs and symptoms. In addition, because the virus continues to be present in the stool for as long as 2-3 weeks after the person recovers, strict hand washing after using the bathroom and before handling food items is important in preventing the spread of this virus. Food handlers who were recently sick can be given different duties in the restaurant so that they do not handle food (e.g., working the cash register).
Recent Activity
News Articles
Latest
- Norovirus cases rising in New Mexico and nationwide (January 3, 2025)
- Increase in Gastrointestinal Illness (November 20, 2015)
Publications
Latest
- Gastrointestinal (GI) Outbreaks Toolkit for Long Term Care Facilities (LTCF) (General)
- Incident Cleaning Poster (Marketing)
- Norovirus Prevention Poster - 2026 (Marketing)
Popular
- Stomach Bug Guide for School Employees (Guide)
- Libro de Bug de Estómago para Empleados de la Escuela (Spanish Version)
- Registered Hospital Disinfectants Effective Against Norovirus (Help)
- Prefilled Specimen Submission Form for norovirus testing (raw stool) (Form)
Resources
Latest
- Birthing Workforce Retention Fund Award Application
- Norovirus Multimedia
- Norovirus Information Video

